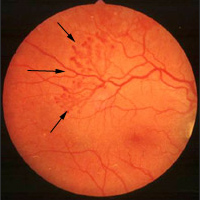
Diabetic Retinopathy
If the blood sugar level of diabetic patients remains at high levels for a long period, disorders will occur in the small blood vessels in the retina, a condition called diabetic retinopathy. Diabetic retinopathy is the main cause of blindness among persons aged 20 to 65 years.